A Safe Space for Nurses to Share Their Coronavirus Fears
Jefferson College of Nursing launches “Nurse2Nurse,” where nurses can debrief with peers.
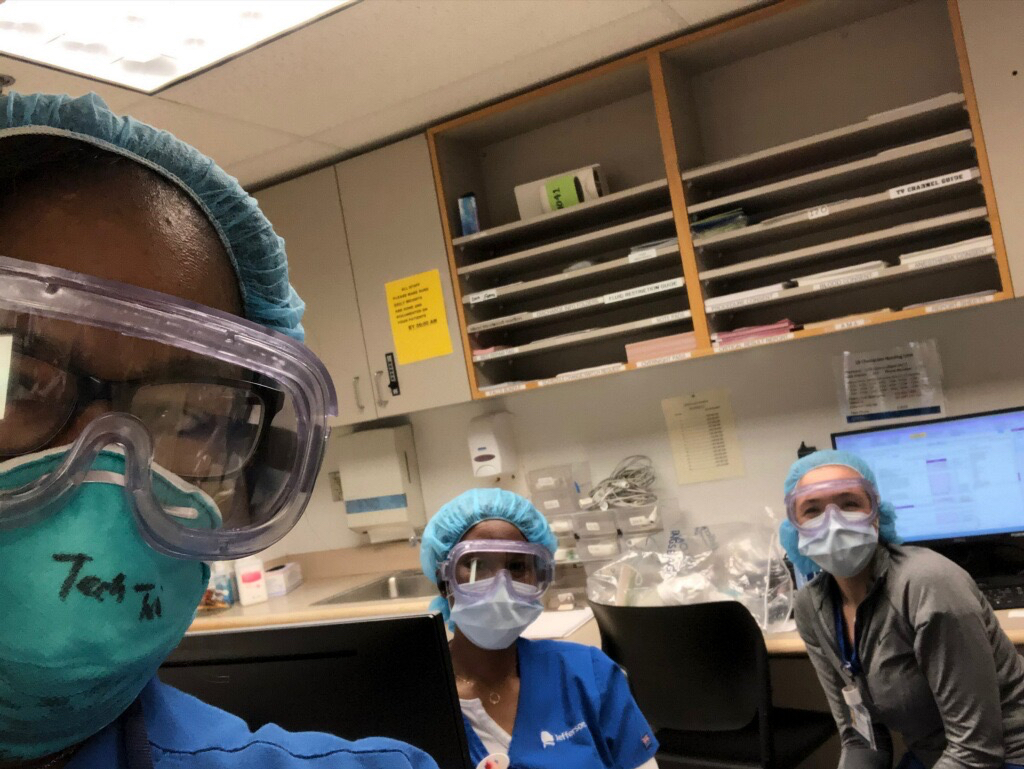
It became clear to anyone who saw the coronavirus “Swab Squad” segment on “The Ellen Show” last month. While Jefferson nurses, along with nurses all over the country, are using social media to relieve the stress of these unprecedented times—many may need someone to talk to about the overwhelming emotions they are experiencing.
In the middle of the Ellen segment, one of the nurses, fighting back tears, talked about having to return to the medical intensive care unit (MICU), what she described as “the epicenter of the COVID-19 positive patients needing critical care.” Surrounded by her colleagues, she told Ellen how it felt. “I was scared. I just reached out in our group chat and said, ‘Hey guys, I’m going to the MICU today, and I’m scared.’ And every single one of them responded immediately, just giving me words of encouragement.”
It will be years before the mental health toll of the COVID-19 pandemic is fully understood, but some early data already paints a bleak picture. A study published March 23 in the medical journal JAMA found that, among 1,257 healthcare workers working with COVID-19 patients in China, 50.4% reported symptoms of depression, 44.6% symptoms of anxiety, 34% insomnia and 71.5% reported distress. Nurses and other frontline workers were among those with the most severe symptoms.
Jefferson leadership had already been working on addressing the emotional needs of frontline staff dealing with the pandemic. Marie Marino, dean of the Jefferson College of Nursing (JCN), put out a call to her faculty to help nurses in particular. Soon, the idea for Jefferson’s “Nurse2Nurse,” a Zoom-based initiative where nurses can debrief with fellow nurses, was born.
A pilot version of the program has recently launched and will expand to the entire health system in the coming weeks. Nurses are invited to join private, 30-minute, one-on-one Zoom calls that accommodate a variety of shifts and times when staff can more easily connect with peers.
The Zoom calls will be fielded by the four JCN faculty members who collaborated on the Nurse2Nurse initiative—Angela Gerolamo, Aparna Kumar, Bobbie Posmontier and Kathryn Shaffer—all veteran nurses experienced and qualified in dealing with crises. Kumar and Posmontier are both psychiatric mental health nurse practitioners, Shaffer is a certified compassion fatigue professional, while Gerolamo, whose expertise is in mental health nursing, will graduate from a psychiatric nurse practitioner program later this month.
“We decided it would be beneficial for nurses to have another nurse to talk to, to be able to share their story with,” Gerolamo says. “It’s like the concept of universality. You want someone who understands what you’re going through and only a nurse can do that.”
The first objective of the Zoom call is to make sure the nurse calling in is safe and not a threat to himself/herself/themselves or others. From there, the call is meant to provide active listening; help the caller become aware of compassion fatigue (characterized by emotional and physical exhaustion leading to a diminished ability to empathize or feel compassion for others) and offer a variety of online Jefferson resources available to staff.
While the number of COVID-19 hospital patients in Philadelphia and its suburban counties in Pennsylvania likely peaked in late April, nurses continue to work long shifts—typically 12-plus hours—under stressful conditions to treat sick patients. Many have witnessed multiple patients die during shifts, under conditions where family members are not permitted to be with their loved ones. All while attempting to avoid contracting the virus, at times isolating themselves from family members to protect others from exposure.
“Right now, these nurses are in what I call warrior mode,” Posmontier says. “You go to work, you take care of patients, you suction them, you give them medication, you give the best care that you can. What I think is going to happen is they’re going to wake up from this adrenaline rush of being in battle and then it’s really going to take an emotional toll.”
The hope is that nurses will use Nurse2Nurse after their shifts—or whenever they feel the need to talk—to help process whatever emotions they may be experiencing. Another 16 volunteers from the nursing faculty have been trained to take Zoom calls from nurses throughout the health system during the designated hours. While volunteers will be able to see who they are speaking with, nurses making the calls are only asked to provide their first names.
It’s casual, it’s not calling employee assistance, it’s not calling a crisis line. It’s just—I need somebody to talk to and a friend might not understand, but we would because we’re all nurses. We get it.
Even before the coronavirus outbreak, 62% of hospital nurses—according to a 2018 RNetwork survey—reported experiencing burnout, a state of emotional and physical exhaustion caused by long periods of stress. That’s an obvious concern, but the brain trust behind Nurse2Nurse is equally concerned about young nurses, many fresh out of college, serving on the frontlines of this pandemic.
“Many of them are very young with little experience, and now they’re going to be seeing people dying on a daily basis or on a shift-by-shift basis,” Shaffer says.
“All of a sudden they’re expected to do these really extraordinary things,” Kumar adds. “Either the patients are sicker or the volumes are much higher than anticipated and there’s likely not as much support for them as there normally would be.”
Jefferson wants its nurses to know that Nurse2Nurse is there for them, with easy access, anonymity and no judgment. “You can just call,” Kumar says. “It’s casual, it’s not calling employee assistance, it’s not calling a crisis line. It’s just—I need somebody to talk to and a friend might not understand, but we would because we’re all nurses. We get it.”